In the intricate world of healthcare, where the well-being of patients hangs in the balance, how do we safeguard against the invisible threats of infection? The answer lies in understanding and meticulously applying isolation precautions a vital strategy that protects both patients and healthcare professionals.
Isolation precautions are not mere protocols; they are the cornerstones of infection control. They are meticulously designed measures implemented to prevent the spread of infectious agents. These measures are adapted based on how the infectious agent is transmitted, ensuring the safety of everyone involved in a patient's care. From the simplest handwashing to the most stringent use of personal protective equipment (PPE), each step is crucial in the fight against the spread of disease. We are dealing with three main types of isolation precautions: contact, droplet, and airborne. Each type dictates the specific measures that must be taken to contain the spread of a particular pathogen. The type of precaution that will be applied depends entirely on the way the infection is transmitted.
| Isolation Precaution Type | Transmission Method | Diseases Examples | Personal Protective Equipment (PPE) | Room Type |
|---|---|---|---|---|
| Contact Precautions | Direct or indirect contact with the patient or their environment | Methicillin-resistant Staphylococcus aureus (MRSA), Vancomycin-resistant Enterococci (VRE), Clostridium difficile (C. diff), and Scabies | Gloves and gown | Private room preferred; cohorting allowed if necessary |
| Droplet Precautions | Droplets generated from coughing, sneezing, or talking | Influenza, Pertussis, Meningitis, and Pneumonia | Surgical mask, gloves | Private room preferred; cohorting allowed if necessary. A mask is also placed on the patient if they need to be transported outside of the room. |
| Airborne Precautions | Airborne particles that can remain suspended in the air for extended periods | Tuberculosis (TB), Measles, Varicella (Chickenpox) | N95 respirator, gloves, gown | Negative pressure room |
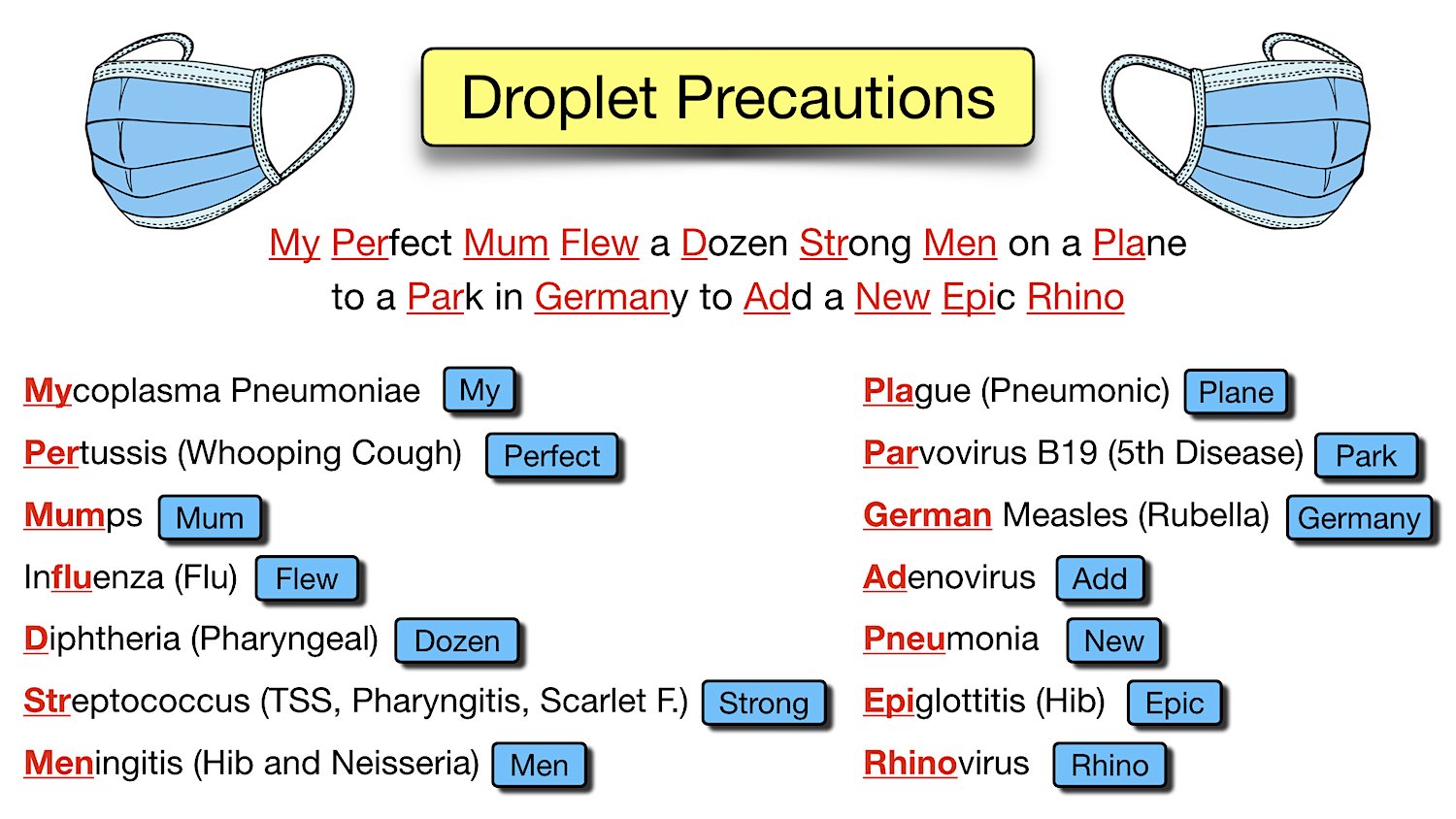
The mnemonic PIMP Pertussis, Influenza, Meningitis, and Pneumonia provides a handy way to remember some of the diseases that necessitate droplet precautions. It's a practical tool that helps healthcare professionals quickly recall the conditions for which this type of isolation is critical. The mnemonic is a valuable resource, allowing for a faster, more efficient application of the appropriate precautions. Similarly, other mnemonics like "MRS. WEE" (MRSA, Respiratory syncytial virus, Skin infections, Wound infections, Enteric infections - Clostridium difficile, Eye infections) are employed for contact precautions and "MTV on Air" (Measles, Tuberculosis, Varicella/Chickenpox) for airborne precautions. Such tools are essential for rapid recall in high-pressure situations.
Contact precautions are often employed in cases of MRSA, VRE, C. diff, and scabies. These precautions prioritize preventing the spread of infections through direct or indirect contact. When coming into contact with a patient under contact precautions, healthcare providers must wear gloves and gowns. The meticulous use of PPE creates a physical barrier, limiting the potential for the transfer of pathogens. Thorough hand hygiene is a constant imperative. It's not merely about following a set of procedures; its about cultivating a mindset of constant vigilance.
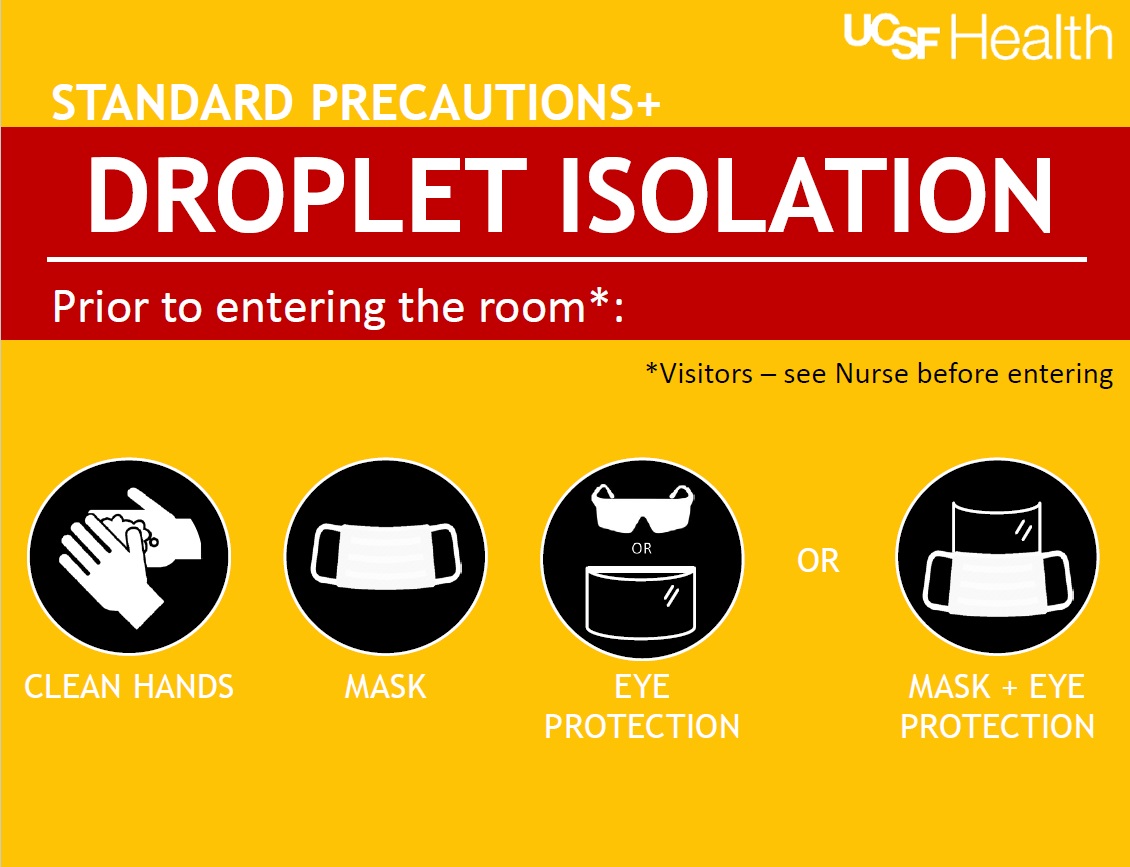
Droplet precautions are designed to address illnesses spread by larger respiratory droplets produced by coughing, sneezing, or even talking. Conditions such as influenza, pertussis, meningitis, and pneumonia fall into this category. For droplet precautions, a surgical mask is required, particularly when within three feet of the patient. Gloves should be worn. The patient should wear a mask while being transported outside the room to minimize the risk of spreading the infection.
Airborne precautions target pathogens that can remain suspended in the air for extended periods and travel over greater distances. These precautions are crucial for diseases like tuberculosis (TB), measles, and varicella (chickenpox). Due to the nature of airborne pathogens, more stringent measures are required. A healthcare worker entering an airborne isolation room must wear an N95 respirator (or a higher-level respirator), gloves, and a gown. The patient is often placed in a negative pressure room. This type of room is designed to draw air away from the hallway, thus preventing the escape of infectious particles into the general environment.
Beyond the technical details, it's vital to consider the psychological impact of isolation on a patient. The initiation of isolation precautions can create feelings of loneliness, anxiety, and even fear. Assessing the patient's emotional response is paramount. Offering emotional support, providing detailed explanations, and regularly updating the patient on their condition and the need for precautions can significantly alleviate these concerns. Limiting patient movement beyond the confines of the room is sometimes necessary to control infection, but clear communication and a compassionate approach can help. Encouraging visitors to wear the appropriate PPE, such as a mask with droplet precautions, provides an additional layer of safety.
The choice of PPE (Personal Protective Equipment) is determined by the type of precaution. For contact precautions, gloves and gowns are essential. Droplet precautions require the use of a surgical mask, along with gloves. Airborne precautions necessitate the highest level of protection: an N95 respirator, gown, and gloves. Its not a matter of "one size fits all." Each piece of PPE serves a specific function in the defense against infection. Proper donning and doffing of PPE are equally critical. Training healthcare professionals on the correct sequence and disposal of PPE is an ongoing effort to limit exposure.
The practical application of these precautions often involves dedicated areas or rooms. Private rooms are generally preferred, especially for contact and droplet precautions, and are mandatory for airborne precautions. Cohorting, the practice of grouping patients with the same infection in the same room, can be an effective method when private rooms are limited. The availability of resources, such as negative-pressure rooms and specialized respirators, directly influences a facility's ability to implement these precautions effectively.
The battle against infection is a continuous one. New pathogens emerge, and existing ones evolve. Healthcare professionals must remain vigilant, continuously updating their knowledge and refining their practices. Staying abreast of the latest guidelines from organizations like the CDC (Centers for Disease Control and Prevention) and the WHO (World Health Organization) is essential. These organizations provide crucial information and training that shape best practices. The emphasis is on being proactive, informed, and ready to adapt to new challenges.
Ultimately, the consistent implementation of isolation precautions is a testament to a healthcare facility's commitment to patient safety. It requires a blend of technical expertise, unwavering dedication, and compassionate care. By understanding the principles, applying the correct practices, and prioritizing patient well-being, healthcare professionals can significantly reduce the risk of infection transmission and contribute to a safer, healthier environment for all.
The fight against infectious diseases is an ongoing process, and each component, from hand hygiene to the correct use of PPE, plays a critical role. The goal is a safer environment for everyone, and the relentless application of these precautions gets us closer to it every day.